Table of Content
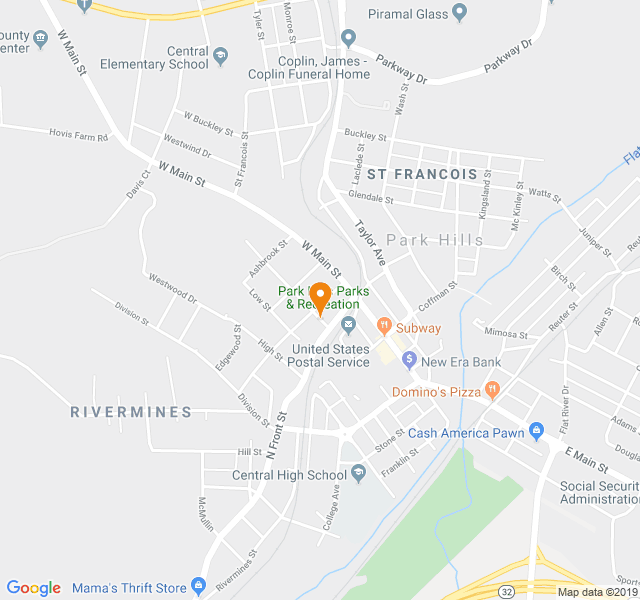
So, we already know that California is the highest paying state for utilization management nurses. But let’s now take a look at the highest-paying metros for utilization management nurses. San Francisco-Oakland-Hayward, CA is the highest paying metro for utilization review nurses. Redding, CA, is the lowest paying metro out of the top ten highest paying metros for utilization nurses. Time management is an important skill to have if you want to be successful in any field. But it is imperative if you are working as a utilization management nurse.

Preparing analysis and reports on significant utilization trends and their impacts on resources is another one of your duties as a utilization management nurse. You will be expected to identify any problems or issues with resource utilization and make recommendations to improve the situation. In some cases, you may also be asked to present your findings to upper management or other key decision-makers. This is an essential part of the job as it can help improve the quality of care and save money for the organization. UR nurses can work in a variety of settings, including hospitals, insurance companies, and government agencies.
Top Cities for Utilization Review Nurses
This includes making sure that patients receive the treatment they need, but also that they aren't receiving care that they aren't eligible for. In these situations, nurses can often feel stressed and frustrated as they try to advocate for their patients while following insurance and facility guidelines. Another one of the pros of being a utilization management nurse is the increased flexibility you'll have in your life.

This means you'll be able to avoid some of the common injuries that nurses often suffer. As Utilization Management Nurse, you will not have to provide hands-on nursing care. You will be working behind the scenes to ensure that patients receive the care they need, while also maximizing the efficiency of the healthcare system. This means that you will not be at an increased risk of infections. In fact, you may even find that your work helps to prevent the spread of diseases.
You will most likely need to earn your bachelor’s degree
Utilization management nurses review patients' records to ensure they meet the coverage requirements. If a patient does not meet the requirements, the nurse works with the provider to determine an alternative plan of care that will be covered. Utilization management nurses also work with patients to educate them about their coverage and help them navigate the claims process. UR nurses are deeply committed to health care quality and patient safety. They help prevent overuse or misuse of medical resources and monitor insurance claims for patients to ensure their medical procedures and services are covered.

You do not have any co-workers to vent to when things get frustrating. 2.Next, you will need to pass the National Certification Licensure Exam (NCLEX-RN). Employee be physically on-site as the work cannot be done from a remote location. The employee is occasionally required to sit and stoop, kneel, or crouch. Working knowledge of MCG criteria and ability to implement and utilize. Self-directed with the ability to adapt in a changing environment.
You’re being taken to an external site to apply.
They work hard to uphold our values and ensure that each patient is taken care of according to their individual needs. To show our appreciation, we work hard to create a supportive and fulfilling environment that helps our employees grow professionally and create long-lasting careers they can take pride in. Depending on the setting in which they work, UR nurses may have different job duties.

As a utilization management nurse, you will be responsible for deciding practices and policies that best ensure effective utilization. In order to do this, you will need to have a strong understanding of the healthcare system and how it works. You will also need to be familiar with the available types of insurance and how they work. Additionally, you will need to be able to effectively communicate with both medical staff and patients. One of the top pros of being a utilization management nurse is that you will not have the same types of stresses you would working bedside. Of course, you will still have some pressure, but it will be more manageable and less intense.
Our packages include health and dental insurances, paid parental leave, retirement program, generous paid time off, and much more! Our comprehensive array of benefits are competitive, affordable, and include choices that meet specific, but ever changing, needs. As Utilization Management Nurse, working from home may not be all cracked up as your thought. Sure, you can wear your comfy clothes and listen to music all day, but big brother is always watching you. Your every move is monitored and reviewed to ensure that you are providing the best possible care for your patients and that you are being productive.

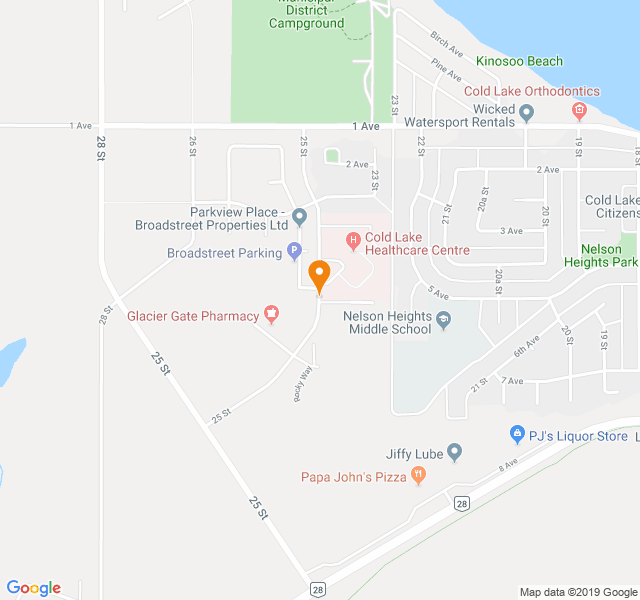
Having a demand in your specific career field is essential to know when you are making plans to enter the workforce. It can be challenging to find a job if there is no demand for your skill set in the current market. Below you will find the reasons why utilization management nurses are in demand. Nursing homes are another setting you may work in as a utilization management nurse.
We recognize that lives may be dependent on our willingness and ability to respond quickly, which is why we strive to understand the special needs of our patients and bring sunshine to their lives. There isn’t one specific certification required to be a UR nurse. Regardless of the setting, all UR nurses are responsible for ensuring that patients receive the care they need in a cost-effective way. UR nurses typically work full-time hours in hospitals, but some may also work in private practices or insurance companies. The goal of utilization review nursing is to maximize the quality of patient care while also minimizing costs.
Jennifer Schlette is a registered nurse in pediatric critical care in New York City. She is the former Director of Undergraduate Nursing at a college located in New York. After obtaining her BSN from the College of Mount Saint Vincent, she went on to complete her MSN. Utilization management specialist does not have to be a nurse.
Glassdoor provides our best prediction for total pay in today's job market, along with other types of pay like cash bonuses, stock bonuses, profit sharing, sales commissions, and tips. Our model gets smarter over time as more people share salaries on Glassdoor. Communicate effectively with individuals outside the company, including clients, medical providers, and vendors. Act as a medical resource in regards to utilization review to Claims Support Nurse, Bill Review, and Claims department. Provide appropriate notices to providers, injured workers, claims staff, and attorneys. Maintains clear, concise, and accurate documentation of requested medical treatments to include clinical findings, treatment guidelines, and determination.
This is because you will not be dealing with sick or injured patients on a daily basis. Instead, you will be working with insurance companies and reviewing medical records. As a utilization management nurse, you will be responsible for coordinating care between various providers. This may involve working with physicians, hospitals, and other health care providers to ensure timely and efficient services. Yes, utilization review nursing can be stressful because the nurse is often in charge of ensuring that patients receive the appropriate level of care.
Access to information is based on a “need to know” and is the minimum necessary to properly perform assigned duties. Use or disclosure shall not exceed the minimum amount of information needed to accomplish an intended purpose. Reasonable efforts, consistent with Albany Med Center policies and standards, shall be made to ensure that information is adequately protected from unauthorized access and modification.